Each minute of our life is a lesson but most of us fail to read it. I thought I would just add my daily lessons & the lessons that I learned by seeing the people around here. So it may be useful for you and as memories for me.
In our current healthcare landscape, the need for a comprehensive overhaul is undeniable. From rising costs and administrative inefficiencies to data privacy concerns, the system is in dire need of transformation. Fortunately, the key to rebuilding a more robust and patient-centric healthcare system lies in placing the power back into the hands of the patients themselves.
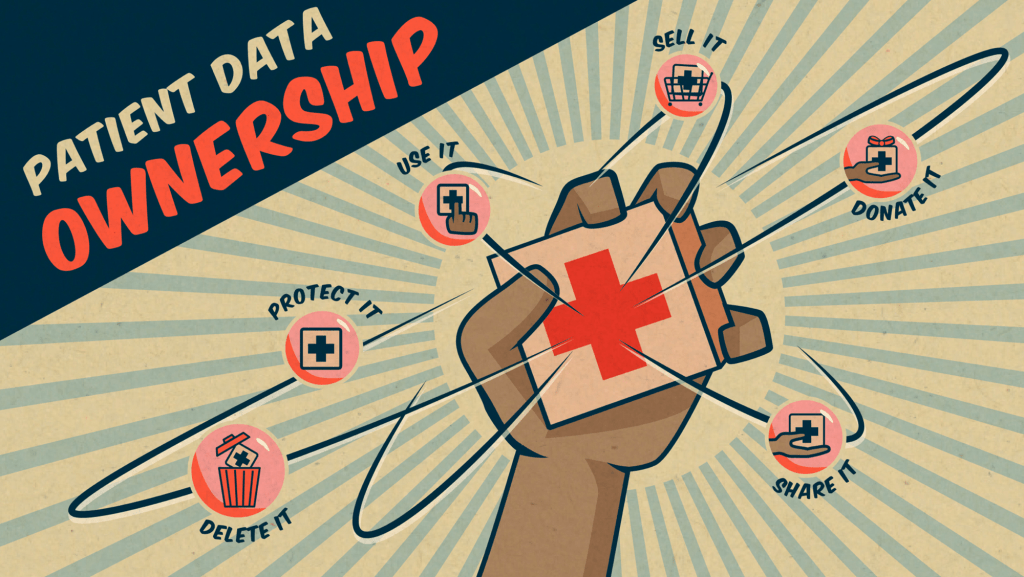
One of the fundamental pillars of this transformation is the idea that patients should have full ownership of their health data. By granting patients the autonomy to access, manage, and share their own data, we can foster a sense of empowerment and engagement that is crucial for their overall well-being. When patients have control over their health data, they become active participants in their care journey, leading to better health outcomes and increased satisfaction with the healthcare process.
Moreover, it is imperative to ensure that patients have complete control over who can access their data and for what purpose. This approach not only safeguards patient privacy but also fosters a sense of trust between patients and healthcare providers. By allowing patients to dictate which providers, applications, and researchers can utilize their data, we can establish a more transparent and collaborative healthcare ecosystem that prioritizes patient preferences and values their consent.

Empowering patients to own their healthcare data is a critical step in enhancing transparency, fostering patient engagement, and promoting personalized care. Here are several key steps that can be implemented to ensure patients have ownership of their data:
- Data Access Portals: Implement user-friendly online portals that allow patients to access their medical records, test results, and treatment history easily.
- Data Download and Sharing Options: Provide patients with the ability to download their health data in a standardized, accessible format, enabling them to share it with other healthcare providers as needed.
- Consent Management Tools: Integrate consent management tools that enable patients to control who can access their data and for what specific purposes, ensuring transparency and privacy protection.
- Patient-Generated Data Integration: Enable patients to contribute data from personal health devices, such as wearable fitness trackers and smartwatches, to create a more comprehensive view of their health status.
- Education and Training Programs: Offer educational resources and training sessions to help patients understand the importance of owning their data, how to access it, and how to utilize it for better self-care and decision-making.
- Data Security Measures: Implement robust security protocols and encryption techniques to safeguard patient data from unauthorized access, ensuring compliance with privacy regulations such as HIPAA (Health Insurance Portability and Accountability Act) and GDPR (General Data Protection Regulation).
- Transparent Data Policies: Establish clear and transparent data policies that outline patients’ rights, data usage guidelines, and procedures for data access, sharing, and revocation of consent.
- Feedback Mechanisms: Create feedback channels where patients can provide input on data management processes, express concerns, and suggest improvements to enhance the overall patient experience and data ownership journey.
- Collaborative Decision-Making Tools: Develop platforms that facilitate collaborative decision-making between patients and healthcare providers, allowing patients to actively participate in treatment planning and goal-setting based on their personal health data.
- Long-Term Data Storage Options: Provide patients with the option to securely store their data for the long term, ensuring accessibility for future reference and continuity of care across different healthcare settings.
By integrating these steps into healthcare systems and practices, patients can take a more proactive role in managing their health, fostering a culture of patient empowerment, and ultimately contributing to the improvement of healthcare outcomes.
In this reimagined healthcare paradigm, the role of data usage and its impact on patient care cannot be overstated. By compensating patients based on how their data is used, we can create a fair and equitable system that acknowledges the value of their contributions. This approach not only incentivizes patients to actively participate in data sharing but also promotes a culture of mutual respect and reciprocity between patients, clinicians, and researchers.
For clinicians, the availability of comprehensive patient data is invaluable in making well-informed decisions and providing high-quality care. With access to a holistic view of a patient’s health history, clinicians can tailor their treatment plans, offer personalized interventions, and proactively address potential health concerns. The integration of patient data into clinical practice not only enhances the efficiency of healthcare delivery but also strengthens the patient-provider relationship, fostering a collaborative and patient-centric approach to care.
The journey towards rebuilding a broken healthcare system is a collective effort that requires the collaboration of healthcare providers, policymakers, and technology innovators. By placing patients at the center of this transformation and empowering them with data ownership and control, we can pave the way for a more inclusive, efficient, and patient-driven healthcare system that prioritizes the well-being and autonomy of every individual.
Through a concerted commitment to patient empowerment, data privacy, and collaborative care, we can lay the foundation for a healthcare ecosystem that not only delivers high-quality care but also fosters a culture of trust, transparency, and patient-centricity. It is time to rebuild our healthcare system, one that truly values and prioritizes the needs and rights of every patient.
Title: Rebuilding the Broken Healthcare System: Empowering Patients with Data Ownership and Control
In our current healthcare landscape, the need for a comprehensive overhaul is undeniable. From rising costs and administrative inefficiencies to data privacy concerns, the system is in dire need of transformation. Fortunately, the key to rebuilding a more robust and patient-centric healthcare system lies in placing the power back into the hands of the patients themselves.

One of the fundamental pillars of this transformation is the idea that patients should have full ownership of their health data. By granting patients the autonomy to access, manage, and share their own data, we can foster a sense of empowerment and engagement that is crucial for their overall well-being. When patients have control over their health data, they become active participants in their care journey, leading to better health outcomes and increased satisfaction with the healthcare process.
Moreover, it is imperative to ensure that patients have complete control over who can access their data and for what purpose. This approach not only safeguards patient privacy but also fosters a sense of trust between patients and healthcare providers. By allowing patients to dictate which providers, applications, and researchers can utilize their data, we can establish a more transparent and collaborative healthcare ecosystem that prioritizes patient preferences and values their consent.
In this reimagined healthcare paradigm, the role of data usage and its impact on patient care cannot be overstated. By compensating patients based on how their data is used, we can create a fair and equitable system that acknowledges the value of their contributions. This approach not only incentivizes patients to actively participate in data sharing but also promotes a culture of mutual respect and reciprocity between patients, clinicians, and researchers.
For clinicians, the availability of comprehensive patient data is invaluable in making well-informed decisions and providing high-quality care. With access to a holistic view of a patient’s health history, clinicians can tailor their treatment plans, offer personalized interventions, and proactively address potential health concerns. The integration of patient data into clinical practice not only enhances the efficiency of healthcare delivery but also strengthens the patient-provider relationship, fostering a collaborative and patient-centric approach to care.
The journey towards rebuilding a broken healthcare system is a collective effort that requires the collaboration of healthcare providers, policymakers, and technology innovators. By placing patients at the center of this transformation and empowering them with data ownership and control, we can pave the way for a more inclusive, efficient, and patient-driven healthcare system that prioritizes the well-being and autonomy of every individual.
Through a concerted commitment to patient empowerment, data privacy, and collaborative care, we can lay the foundation for a healthcare ecosystem that not only delivers high-quality care but also fosters a culture of trust, transparency, and patient-centricity. It is time to rebuild our healthcare system, one that truly values and prioritizes the needs and rights of every patient.
Join me in revolutionizing the future of healthcare. Together, we can create a system that prioritizes transparency, efficiency, and patient well-being.
If you wanna share your experiences, you can find me online in all your favorite places LinkedIn and Facebook. Shoot me a DM, a tweet, a comment, or whatever works best for you. I’ll be the one trying to figure out how to read books and get better at playing ping pong at the same time.

